Bladder Cancer
Kidney Cancer :: Bladder Cancer
High Stage Bladder Cancer
 |
| Female |
Introduction
Cancer of the bladder is the fourth most common cancer among men and the ninth most common cancer among women. About 2,000 men and 1,000 women will develop bladder cancer this year in Australia. There will be 250,000 new cases of bladder cancer world wide. Bladder cancer is the fourth leading cause of cancer and the seventh leading cause of cancer death. Cancer of the bladder may occur at any age, but it usually strikes those over 50 years old.
If it were to be detected and treated early, bladder cancer is almost always cured (the 5-year survival rate of early bladder cancer is 90%). About 85% of all bladder cancer is of low grade and stage at the time of diagnosis. Unfortunately about 15% of patients with bladder cancer will have high grade or high stage lesions at the time of diagnosis. If bladder cancer has spread from the bladder by the time of diagnosis, less than one in ten patients survive five or more years. Each year about 550 men and 300 women die of the disease in Australia. During the past 30 years, the death rate for bladder cancer has declined slightly for men but more so for women. This success is attributed to earlier detection and better treatment options.
What the Bladder does
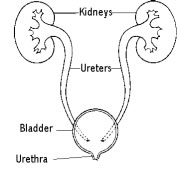
The bladder is a muscular sac that collects and stores urine. It is hollow and its shape depends on how much urine it holds. When it is empty it looks like a deflated balloon. As it fills, it becomes rounded and pushes up against the abdomen.
Urine is made up of water and wastes removed from the blood. Urine is created by filtering the blood in the kidneys. The urine then travels down tubes known as ureters and is stored in the bladder until it can be released from the body through another tube, the urethra.
The bladder is lined by special cells, called transitional cells. These cells are unique in that they have the ability to expand and deflate, which makes sense as the bladder fills and empties urine. Almost all bladder cancers arise in this lining layer. These cancers in time can grow and spread into the underlying bladder muscle. Cancers originating in the bladder muscle are very rare.
What is Cancer?
Cancer is a disease caused by the abnormal growth of cells. Cancer can occur in any part of the body. Normally the cells that make up the different parts of the body divide and reproduce in an orderly manner, so that we can grow tissue, replace worn-out body tissue, and repair injuries. Sometimes, however, cells get out of control, divide more than they should, and form masses known as tumours.
Some tumours may interfere with body functions and need to be removed, but do not spread to other parts of the body. These are known as benign tumours.
Malignant, or cancerous tumours, not only invade, destroy or replace normal body tissue, but individual cancerous cells break away from the original tumour and spread through the blood stream and lymph channels (lymph nodes) to other parts of the body. There they may form additional malignant tumours. This process is known as metastasising and the new tumours are called metastases. Only a pathologist can make a diagnosis of cancer by looking at biopsy specimens of the tumour. In addition to telling whether or not a tumour is cancerous or benign, the pathologist may also be able to tell the treating physician how aggressive or rapidly growing a cancer might be. How aggressive the tumour looks when examined under the microscope is called the"grade". High grade cancers grow faster and spread to other areas more quickly and earlier. Low grade cancers grow slower and spread later.
If bladder cancer spreads, it usually goes first to the lymph nodes in the pelvis. Bladder cancer also tends to spread to the lungs, liver, and bones.
Types of Bladder Cancer
Bladder cancers must be classified in three different ways - Type, Grade and Stage. Knowing the cell type, grade and stage of bladder cancer is essential in planning the right treatment.
Type
Bladder cancers are classified according to the type of cell that has become cancerous. About 90% of cancers of the bladder involve transitional cells. Transitional cells are merely the name of the usual cell that lines the bladder wall. Transitional cells are unique to the urinary tract and line the kidneys and ureters as well. Other types of cells that are found less frequently in bladder cancer include squamous cell cancers or adenocarcinomas.
Transitional-cell cancers of the bladder can be further divided into 'papillary', 'solid' tumours and 'carcinoma-insitu' (CIS).
Papillary, which means 'finger-like', are usually low grade tumours. This means that they grow slowly.
Papillary tumours also usually grow towards the inside of the bladder, not towards the muscle lining.
Sometimes, particularly if untreated, papillary tumours will invade into the bladder muscle and then spread into the body. Papillary tumours occur more than twice as often as solid tumours. There may be one papillary tumour or several. Patients with tumours in multiple areas are more likely to have the cancer come back, or recur, after treatment. In general, papillary cancers of the bladder have a recurrence rate of up to 70%, meaning that even if all the cancer is removed, new cancers will develop in other parts of the bladder in 7 of 10 patients at a later time. These recurrences can occur at any time, but usually within two years.
Solid tumours are rarer but tend to be more aggressive, recur more often, and have a tendency to invade deeply into the bladder wall at an earlier stage.
Carcinoma in situ (CIS) is a unique situation. CIS is a very aggressive looking cancer, but involves only the innermost cells lining the bladder. It may occur diffusely throughout the bladder or in small areas. CIS does not look like a tumour, but more like a flat red area on the bladder wall. It is often associated with symptoms similar to a bladder infection, such as pain and or burning with urination and urinary frequency. CIS is associated with a high rate (more than 50%) of developing invasive, usually solid, bladder cancers within 5 years if not treated.
Grade
The GRADE is defined by the pathologist from the bladder biopsy. The grade gives us an idea of how fast the cancer might be growing or how aggressive it might be. High grade cancers grow faster and spread earlier than low grade cancers. The current system of grading uses only three different grades: well-differentiated (Grade I), moderately differentiated (Grade II), and poorly differentiated (Grade III). It is still used in general discussions about cancer. Some pathologists will use a 4-level grading system, I, II, III and IV. Either system is acceptable. The pathologist will always note how many levels they use by declaring the cancer as a II/III or II/IV. The denominator or second number states what system they use.
Well-differentiated means the cancer has more resemblance to normal bladder tissue and therefore usually does not grow or spread quickly. Poorly differentiated tumours do not resemble normal bladder and usually grow quickly and spread to other tissues earlier. Moderately differentiated are in the middle.
Stage
Stage is defined as the estimation of extent (size and location) of the cancer at the time of diagnosis. More specifically, stage how extensive is the cancer within the bladder and if it has spread to tissues around the bladder, or to other parts of the body.
The first important part of the stage of the tumour to define is the 'local' stage or how extensively the tumour has infiltrated into and/or around the bladder. The bladder wall has four layers. The innermost lining of the bladder (called the endothelium) is made up of specialised cells called transitional cells – it is from these transitional cells that 95% of bladder cancers originate. Underneath the epithelium is a special layer called the 'lamina propria'. Then comes the muscle layer of the bladder. The outermost layer is called the serosa and is comprised mostly of fat. The deeper the invasion the more likely a tumour will recur at a later time and also spread to other organs - a situation called 'metastases'.
In some patients suspicion of spread of the cancer may exist. This situation occurs primarily in patients with higher grade cancers that have invaded deeply into the bladder, particularly the bladder muscles. In those patients we may elect to do 'staging studies' looking for spread of the cancer. The studies vary from patient to patient depending on various factors. The usual initial staging studies include the pathology report from the initial biopsy, the general physical examination and digital rectal examination, and a CT scan of the chest, abdomen and pelvis. Special scans, such as bone scans, may also be suggested. The stage of the cancer is the most important deciding factor in which treatment will be used.
Who is at risk of developing bladder cancer?
The relationship between bladder cancer and smoking was suggested first in 1895. With this report, bladder cancer was one of the first cancers for which 'carcinogens' (cancer causing substances) were found to play a role in causing the disease. Smokers are three times as likely to develop bladder cancer as nonsmokers. Three out of every five cases of bladder cancer is linked to smoking. This link between smoking and bladder cancer is especially strong among men.
Bladder cancer is more common in highly industrialized areas and among workers exposed to certain chemicals. Certain aniline derivatives, benzidine, 2-napthylamine, and other chemicals used in dye manufacturing increase the risk to workers involved in the process. Painters and workers in the rubber, metal, textile, and leather industries are also at high risk.
The artificial sweeteners saccharin and cyclamates have been shown to cause bladder cancer in rats when given in very large doses. The link between these sweeteners and bladder cancer in humans has not been shown.
In the Middle East and Africa, certain parasitic worm infections have been linked with bladder cancer.
Signs and Symptoms
Blood in the urine is usually the first sign of bladder cancer. Many times, blood in the urine cannot be noticed by the individual, but is found by urine analysis done as part of a regular checkup or treatment for another medical condition. If blood can be seen in the urine, it may change the colour of the urine from yellow to smoky to rusty to bright red. The blood may disappear for days or even weeks, only to reappear. Blood in the urine can be caused by a number of medical problems besides cancer. These include infection, benign tumours, kidney stones and a number of kidney diseases. If blood is noticed, a doctor should be consulted to determine its cause.
Early stage bladder cancer does not usually cause pain, but pain may sometimes occur along with the bleeding.
The need to urinate may seem more urgent and frequent. Signs of late stage bladder cancer may include all of the above plus possible bowel problems, loss of appetite, and weight loss. Pain may be felt in the lower back and in the bones.
How the diagnosis is made
The diagnosis of bladder cancer begins with a complete medical history. The doctor will ask questions about the patient's overall health and bladder cancer risk factors, such as smoking and exposure to certain industrial
chemicals. To determine if cancer is present, some or all of the following tests may be done:
Urinalysis is the analysis of the physical and chemical properties of a sample of urine. As part of the
diagnostic workup for bladder cancer, it can reveal blood in the urine in amounts too small to be noticed by the patient, or can confirm that blood is still in the urine.
Intravenous Pyelogram (IVP) can help determine the source of the bleeding. A small amount of
special X-ray dye is injected into the bloodstream. This dye is quickly absorbed by the kidneys. X-rays are then taken to track the dye as it makes its way through the urinary system. The images displayed on the X-rays can help locate tumours and other sources of bleeding.
Cystoscopy permits the doctor to actually look inside the bladder. A small slender tube, the cystoscope, is inserted into the bladder through the urethra, the final portion of the urinary system. The cystoscope is fitted with a lens and a light which allows the doctor to carefully examine the inner surface of the bladder and look for any abnormal areas. This is usually done in the doctor's office using a local anaesthetic. The procedure takes only a few minutes to perform.
Resection and Biopsy is the removal and examination under a microscope of suspicious looking areas from the bladder. The cells are removed through the cystoscope or telescope. These procedures are usually
performed in the hospital with an anaesthetic. Since bladder cancer may be present in more than one area of the bladder, several samples of bladder--from both normal and abnormal looking areas--will be removed for examination. Only a biopsy can tell for sure whether cancer is present. The biopsies from areas that do not have cancer (called 'random biopsies') will often give valuable information about the long-term chances of cancer recurrence.
BTA Test is a new urine test that is able to indicate in many cases the presence of bladder cancer cells. The BTA is done on a voided urine specimen and can be done quickly in the doctor's office or laboratory. BTA is able to detect unique proteins (or antigens) that many bladder cancers produce.
Cytology is the study of individual cells. The inside of the bladder is irrigated with a salt-water solution. The cells suspended in the solution are examined for any abnormalities. PAP smear is an example of cytology when we look at scrapings from the female cervix.
Bimanual Abdominal and Rectal Examination lets the doctor feel for any hard areas in part
of the bladder. The doctor inserts a gloved finger into the vagina or rectum and then presses down gently on the abdomen. A hardened spot that can be felt may be a sign of a tumour.
Surgery
Surgery For Early or Superficial Bladder Cancer
Most early bladder cancers are biopsied and removed through an endoscope, a thin telescopic tube inserted into the urethra and then into the bladder. This is usually referred to as 'transurethral resection'. This type of removal is effective for those cancers, usually the papillary type, which have NOT invaded into the bladder muscle. An electric cutting knife 'or loop' attached to the endoscope is used to remove the tumours. In some instances, lasers, or very intense light beams, are being used to destroy bladder tumours. Several tumours may be removed during a single operation and the procedure can be repeated as often as necessary. An anaesthetic, such as general anaesthesia or spinal, is necessary for any transurethral resection.
Surgery for Advanced or Deep Bladder Cancer
Patients with more advanced disease, that which has grown into the bladder muscle or into the lamina propria, often need to have the bladder removed, a procedure known as a total or radical cystectomy. This of course means that the urine must be diverted away from the bladder. Options for diversion are discussed below.
Patients who have had superficial bladder tumours removed transurethrally and, despite further treatment, continue to develop many tumours scattered over the lining of the bladder are at high risk of developing invasive cancer and having it spread to other parts of the body. For that reason these patients may also have a total cystectomy.
In very rare select cases where the cancer cells have invaded deep into the bladder wall, but only in a limited part, a partial cystectomy can be done. This spares enough bladder so that the urine does not need to be diverted.
When doing a total cystectomy for cancer in women, the uterus, ovaries, fallopian tubes, part of the vagina, and urethra are usually removed.
Urinary Diversion After Total Cystectomy
Once the bladder is removed, the patient needs another way pass urine out of the body. This is known as urinary diversion and many options are available.
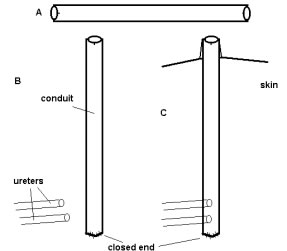
Ileal conduit or urostomy
The ureters can be rerouted or diverted to a tube made from a piece of the small intestine or ileal conduit. A piece of small intestine with its blood supply attached is separated from the main flow of the bowel contents.
This piece is connected on one end to the ureters and on the other end to an opening made on the outside of the body, usually to the right and below the belly button. The opening created is called a stoma. A disposable bag is then attached over the opening on the outside of the body. Before leaving the hospital, the patient learns how to change the bag and how to clean and take care of the stoma.
- Separate a segment of intestine, reconnect remaining intestine
- Close end of urinary conduit
- Attach ureters near closed end of conduit. Attach opposite end of conduit to skin.
Continent Diversion and Neobladder
A long piece of intestine, can also be used to construct a new bladder. Small intestine, or colon or both are used to construct neobladders or continent diversions.
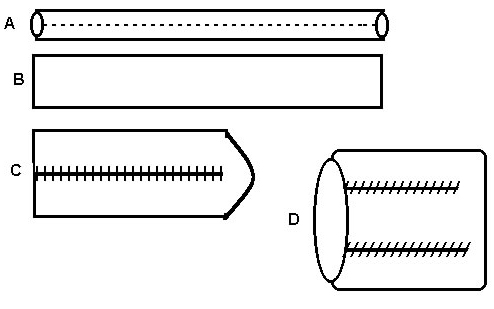
Neobladder
In patients in whom the urethra is still intact, the neobladder and urethra are reattached and the urinary system works much as it did before.
- Separate a segment of intestine, reconnect remaining intestine
- Open the segment of intestine on one side
- Fold and sew the intestine to double the width
- Fold and sew the intestine in opposite direction to make a pouch
- Align the pouch with the urethral opening
- Sew the pouch to the urethra
Neobladder
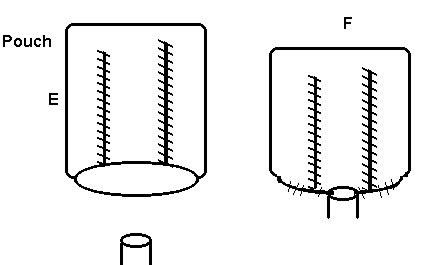
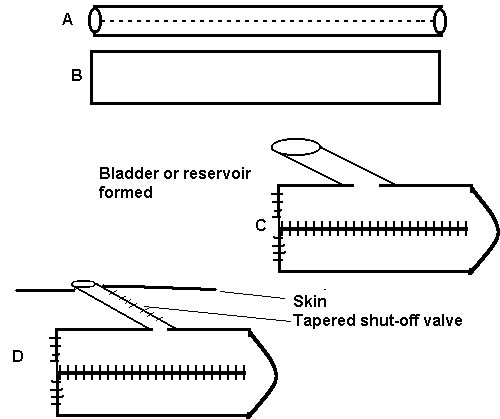
Continent Diversion
In patients in whom the urethra needs to be removed, reattachment to the urethra is impossible. In these cases, the 'neobladder' is brought up to the abdomen with a special non-leaking valve so that urine does not leak out.
This requires the patient to pass a small rubber tube into the neobladder every 4-6 hours to empty the stored urine.
Creating and putting in place a neobladder to the urethra provides more comfort and ease to patients than having a stoma or bag and comes close to returning the bodily functions to normal.
Creating and putting in place a neobladder to the abdomen (continent diversion) provides more cosmetic appeal to the patient than having a urinary bag. Before the bladder is removed, the patient should discuss with the doctor what will be done to divert the urine and what effect it could have on the patient's lifestyle.
- Separate a segment of intestine, reconnect remaining intestine
- Open the segment of intestine on one side
- Fold and sew the intestine to double the width and close end to make a pouch
- Taper skin conduit to create a water-tight valve and connect to skin
Continent Diversion
Chemotherapy
Intravesical Chemotherapy
(Intra = into, vesical = bladder, chemo = chemical)
Intravesical chemotherapy refers to chemical treatments that are instilled into the bladder through the urethra using a catheter or rubber tube. These procedures are usually done in the office and require only 5 minutes to perform. The tube is removed immediately, but the medications must be kept in the bladder for about two hours.
Most commonly, intravesical chemotherapy is used for patients whose tumours have been completely removed but who are at high risk of having recurrences or new tumours develop at a later time. On occasion, intravesical chemotherapy is used to treat multiple bladder tumours that could not be completely removed by surgery.
Chemotherapy given directly into the bladder does not usually cause side effects like chemotherapy taken orally or injected into the body. Because the therapy is limited to the bladder most of the side-effects are the irritative effects on the bladder, such as frequency, urgency and burning with urination. Most of these effects dissipate after the treatments are discontinued. The frequency and duration of treatments vary with different medications.
Currently used drugs include names such as BCG, Thio-Tepa, Mitomycin-C and Adriamycin Adriamycin. Each has unique properties and side effects which will be discussed by your urologist before use.
Systemic Chemotherapy
Chemoprevention For Early Bladder Cancer
In patients with early bladder cancer (not invading muscle), some reports have suggested that megadoses of vitamins A, B6, C and E and zinc can be helpful in reducing recurrences. These reports are early and have yet not been substantiated in multi-center trials. The doses used included vitamin A -- 40,000 units, B6 -- 100mg, C -- 2,000 mg, E -- 400 units and zinc 90mg. These are taken in divided doses twice a day. For the most part, these doses are safe, although vitamin A in higher doses can cause liver problems and some patients have stomach upset with any vitamin preparation. Until we have more experience, vitamin supplementation to other treatment must be regarded as experimental.
Systemic Chemotherapy For Advanced Disease
Systemic chemotherapy means that the medication is allowed to enter the blood stream, either by injection or by ingestion. These are medications that have the ability to kill cells that are multiplying quickly such as cancer cells. Many normal body cells also multiply quickly and can be harmed as well. Hopefully, the strong drugs used in systemic chemotherapy will cause more damage to cancer cells than to normal cells.
Some of the rapidly dividing cells systemic chemotherapy can harm include those of the bone marrow, hair and those lining the stomach. That is why systemic chemotherapy often causes anaemia, bleeding, hair loss, nausea and vomiting, increased likelihood of developing infections and mouth sores. Most of these side effects disappear once treatment is stopped. Since each person reacts differently to treatment, the side effects will differ.
The doctor, usually a Medical Oncologist, must be very careful about how large the dose is and how often it is given.
Studies are now going on to see if giving systemic chemotherapy before or after removing the bladder (total cystectomy) could improve survival results. This idea is still being tested and the treatments are experimental only.
Radiation
The aim of radiation therapy is to destroy cancer cells by injuring their ability to divide, while causing the least amount of damage possible to other cells. Radiation may be used to help shrink bladder tumors before removal, to destroy any cancer cells remaining after surgery, and to relieve pain for patients not healthy enough to have surgery. It may also be used as the only treatment for patients not able to endure cystectomy and chemotherapy.
New studies suggest that combined radiation and chemotherapy might be better than cystectomy for some patients. Other studies are looking at the combined use of surgery, chemotherapy, and radiation to control tiny pockets of metastatic disease among patients with advanced bladder cancer. Both these approaches are still considered experimental.
Side effects of radiation include skin changes, nausea and vomiting, and a tired or sluggish feeling. These generally go away once treatment is stopped.
Support for The Patient
Providing the best care for the patient means not only treating the cancer, but easing the side effects and all the physical and emotional strains. This calls for a teamwork approach among the surgeon, the doctors who will plan radiation and chemotherapy, the pharmacists, nurses, social workers, and other health care workers.
Dietitians can help patients make any needed dietary changes so that their nutritional needs are met during and after treatment. Nurses often provide emotional support and teach the patient and other members of the family"do's and don'ts" of home health care. Patients whose bladders had to be removed and who pass urine through a stoma can get help and advice on cleaning and taking care of the stoma from a stoma therapist.
Radical surgery and radiation can impair sexual function. A women who has had part of her vagina removed may have it reconstructed using tissue from the intestine. Any loss of sexual function can cause emotional distress and an understanding and supporting partner can help the patient through this difficult time.
Psychological counselling can help patients and family members to cope with the disease and its effects on their lives. Patients and family members may find it helpful to join a group offering emotional support and advice on coping with bladder cancer.
Patients and family members should stay actively involved in choosing the right treatment. They have a right to know everything about the treatment and should ask questions.
Follow-Up Care
Follow up depends on the stage and type of disease that is being treated.
For patients with superficial bladder cancers that are removed with telescopic surgery, urinalysis and cystoscopy should be done on a regular basis usually every three to four months for the first year and then less often, but at least once a year in the consecutive years. Based on the results of cystoscopy and BTA testing or cytology, further tests may be ordered.
For patients after total cystectomy for advanced disease, frequent follow-up examinations are needed to see if the disease has recurred or spread to other parts of the body. These exams should be done every three to six months during the first three years after treatment. Most bladder cancers that recur do so during the first three years.
Patients whose bladders have been removed will be examined to see if the rest of the urinary system is disease free and if the urinary diversion is working properly.
Expected Survival Times
The outlook for patients for early-stage bladder cancer that has not invaded the bladder wall is very good. About 90% of those patients live for five or more years with localized diagnosis and treatment. For patients whose cancer has spread to areas near the bladder, the 5 year survival rate is 45%. For those with advanced disease that has spread far from the bladder, the 5-year survival rate is 10%.
How To Help Guard Against Bladder Cancer
- Don't smoke. If you do, make plans to quit right away. If you need help in quitting, call the Quit
helpline
- As part of your overall defense against cancer, have regular medical checkups.
- If you notice blood in your urine, or any other change in bladder habits, see your doctor.
Treating The Disease
Surgery, alone or combined with other therapies, is used to treat more than 90% of bladder cancer patients.
Radiation and chemotherapy can increase the chances for a cure, help control metastatic disease, and prevent the disease from recurring, but are usually not used as the main or only treatment.
Surgery
Surgery for Early or Superficial Bladder Cancer
Most early bladder cancers are biopsied and removed through an endoscope, a thin telescopic tube inserted into the urethra and then into the bladder. This is usually referred to as 'transurethral resection'. This type of removal is effective for those cancers, usually the papillary type, which have NOT invaded into the bladder muscle. An electric cutting knife 'or loop' attached to the endoscope is used to remove the tumours. In some instances, lasers, or very intense light beams, are being used to destroy bladder tumours. Several tumours may be removed during a single operation and the procedure can be repeated as often as necessary. An anaesthetic, such as general anaesthesia or spinal, is necessary for any transurethral resection.
Chemotherapy
Intravesical Chemotherapy
(Intra = into, vesical = bladder, chemo = chemical)
Intravesical chemotherapy refers to chemical treatments that are instilled into the bladder through the urethra using a catheter or rubber tube. These procedures are usually done in the office and require only 5 minutes to perform. The tube is removed immediately, but the medications must be kept in the bladder for about two hours.
Most commonly, intravesical chemotherapy is used for patients whose tumours have been completely removed but who are at high risk of having recurrences or new tumours develop at a later time. On occasion, intravesical chemotherapy is used to treat multiple bladder tumours that could not be completely removed by surgery.
Chemotherapy given directly into the bladder does not usually cause side effects like chemotherapy taken orally or injected into the body. Because the therapy is limited to the bladder most of the side-effects are the irritative effects on the bladder, such as frequency, urgency and burning with urination. Most of these effects dissipate after the treatments are discontinued. The frequency and duration of treatments vary with different medications.
Currently used drugs include names such as BCG, Thio-Tepa, Mitomycin-Cand Adriamycin. Each has unique properties and side effects which will be discussed by your Urologist before use.
Systemic Chemotherapy
Chemoprevention For Early Bladder Cancer
In patients with early bladder cancer (not invading muscle), some reports have suggested that megadoses of Vitamins A, B6, C and E and Zinc can be helpful in reducing recurrences. These reports are early and have not been substantiated in multi-center trials as of yet. The doses used included Vitamin A -- 40,000 units, B6 -- 100mg, C -- 2,000 mg, E -- 400 units and Zinc 90mg. These are taken in divided doses twice a day. For the most part, these doses are safe, although Vitamin A in higher doses can cause liver problems and some patients have stomach upset with any vitamin preparation. Until we have more experience, vitamin supplementation to other treatment must be regarded as experimental.
Support for The Patient
Providing the best care for the patient means not only treating the cancer, but easing the side effects and all the physical and emotional strains. This calls for a teamwork approach among the surgeon, the doctors who will plan radiation and chemotherapy, the pharmacists, nurses, social workers, and other health care workers.
Dietitians can help patients make any needed dietary changes so that their nutritional needs are met during and after treatment. Nurses often provide emotional support and teach the patient and other members of the family"do's and don'ts" of home health care. Patients whose bladders had to be removed and who pass urine through a stoma can get help and advice on cleaning and taking care of the stoma from a stoma therapist.
Psychological counselling can help patients and family members to cope with the disease and its effects on their lives. Patients and family members may find it helpful to join a group offering emotional support and advice on coping with bladder cancer.
Patients and family members should stay actively involved in choosing the right treatment. They have a right to know everything about the treatment and should ask questions.
Follow-Up Care
Follow-up depends on the stage and type of disease that is being treated.
For patients with superficial bladder cancers that are removed with telescopic surgery, urinalysis and cystoscopy should be done on a regular basis usually every three to four months for the first year and then less often, but at least once a year in the consecutive years. Based on the results of cystoscopy and BTA testing or cytology, further tests may be ordered.
Expected Survival Times
The outcome of patients with early-stage bladder cancer that has not invaded the bladder wall is very good. About 90% of these patients live for five or more years with localised diagnosis and treatment.
What's New
Much of the research on bladder cancer is aimed at DNA, the genetic information inside the cancer cells. Many cancer cells have DNA abnormalities these may used to identify more cancers that need to be treated more aggressively. In addition, some of these DNA tests may help identify pre-cancerous conditions that cannot be identified with current techniques. The most common of the DNA markers include p53, Ki 67, Cyclin D1, Gactin.
How to Help Guard Against Bladder Cancer
- Don't smoke. If you do, make plans to quit right away. If you need help in quitting, call the Quit Helpline.
- As part of your overall defense against cancer, have regular medical checkups.
If you notice blood in your urine, or any other change in bladder habits, see your doctor. |
